Search
- Page Path
- HOME > Search
Original Article
- Thyroid
Thyroid Cancer Screening - Cost-Utility Analysis of Early Detection with Ultrasonography of Differentiated Thyroid Cancer: A Retrospective Study on a Korean Population
- Han-Sang Baek, Jeonghoon Ha, Kwangsoon Kim, Ja Seong Bae, Jeong Soo Kim, Sungju Kim, Dong-Jun Lim, Chul-Min Kim
- Endocrinol Metab. 2024;39(2):310-323. Published online April 9, 2024
- DOI: https://doi.org/10.3803/EnM.2023.1870
- 976 View
- 11 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
There is debate about ultrasonography screening for thyroid cancer and its cost-effectiveness. This study aimed to evaluate the cost-effectiveness of early screening (ES) versus symptomatic detection (SD) for differentiated thyroid cancer (DTC) in Korea.
Methods
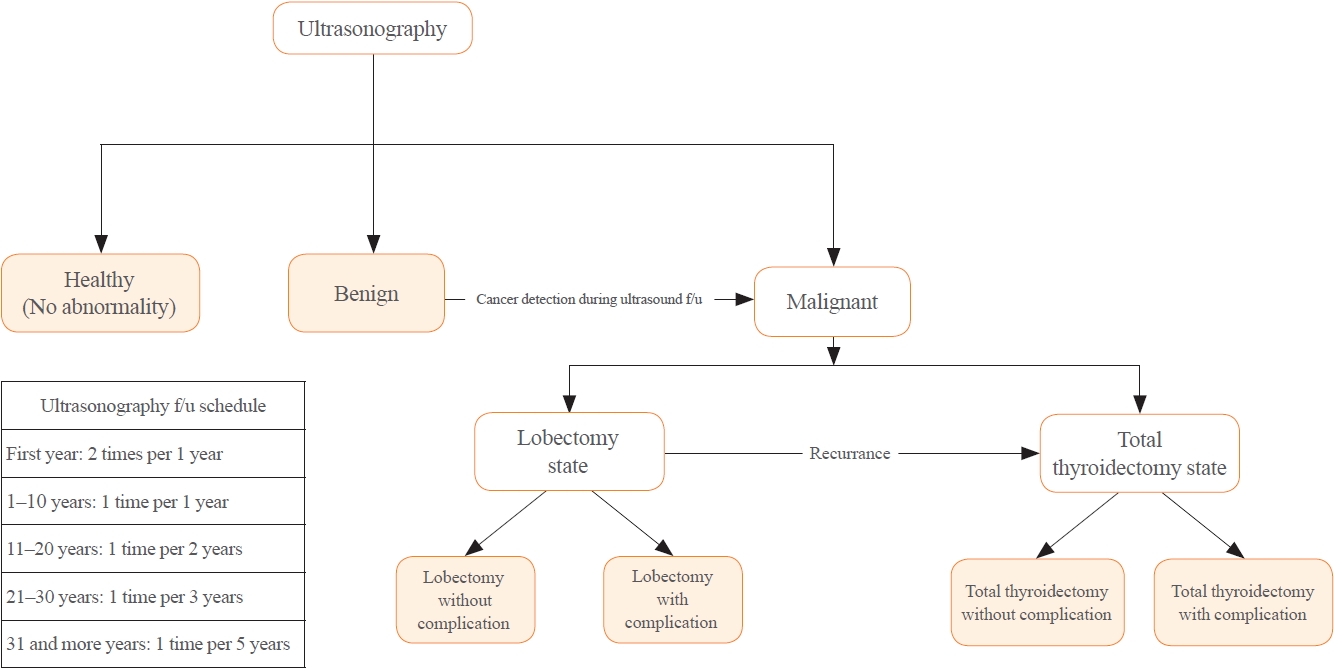
A Markov decision analysis model was constructed to compare the cost-effectiveness of ES and SD. The model considered direct medical costs, health outcomes, and different diagnostic and treatment pathways. Input data were derived from literature and Korean population studies. Incremental cost-effectiveness ratio (ICER) was calculated. Willingness-to-pay (WTP) threshold was set at USD 100,000 or 20,000 per quality-adjusted life year (QALY) gained. Sensitivity analyses were conducted to address uncertainties of the model’s variables.
Results
In a base case scenario with 50 years of follow-up, ES was found to be cost-effective compared to SD, with an ICER of $2,852 per QALY. With WTP set at $100,000, in the case with follow-up less than 10 years, the SD was cost-effective. Sensitivity analysis showed that variables such as lobectomy probability, age, mortality, and utility scores significantly influenced the ICER. Despite variations in costs and other factors, all ICER values remained below the WTP threshold.
Conclusion
Findings of this study indicate that ES is a cost-effective strategy for DTC screening in the Korean medical system. Early detection and subsequent lobectomy contribute to the cost-effectiveness of ES, while SD at an advanced stage makes ES more cost-effective. Expected follow-up duration should be considered to determine an optimal strategy for DTC screening.

Letter
- Thyroid
- Re-Increasing Trends in Thyroid Cancer Incidence after a Short Period of Decrease in Korea: Reigniting the Debate on Ultrasound Screening
- Chan Kwon Jung, Ja Seong Bae, Young Joo Park
- Endocrinol Metab. 2022;37(5):816-818. Published online October 11, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1586

- 1,776 View
- 166 Download
- 3 Web of Science
- 5 Crossref
-
 PDF
PDF PubReader
PubReader  ePub
ePub -
Citations
Citations to this article as recorded by- Bilateral axillo-breast approach robotic total thyroidectomy without isthmectomy: a case report
Hyeji Kim, Hyeonuk Hwang, Hyungju Kwon
The Ewha Medical Journal.2024;[Epub] CrossRef - Contents analysis of thyroid cancer-related information uploaded to YouTube by physicians in Korea: endorsing thyroid cancer screening, potentially leading to overdiagnosis
EunKyo Kang, HyoRim Ju, Soojeong Kim, Juyoung Choi
BMC Public Health.2024;[Epub] CrossRef - Survival Comparison of Incidentally Found versus Clinically Detected Thyroid Cancers: An Analysis of a Nationwide Cohort Study
Shinje Moon, Eun Kyung Lee, Hoonsung Choi, Sue K. Park, Young Joo Park
Endocrinology and Metabolism.2023; 38(1): 81. CrossRef - Cumulative exposure to metabolic syndrome increases thyroid cancer risk in young adults: a population-based cohort study
Jinyoung Kim, Kyungdo Han, Mee Kyoung Kim, Ki-Hyun Baek, Ki-Ho Song, Hyuk-Sang Kwon
The Korean Journal of Internal Medicine.2023; 38(4): 526. CrossRef - Cost-Effectiveness of Active Surveillance Compared to Early Surgery of Small Papillary Thyroid Cancer: A Retrospective Study on a Korean Population
Han-Sang Baek, Jeonghoon Ha, Kwangsoon Kim, Jaseong Bae, Jeong Soo Kim, Sungju Kim, Dong-Jun Lim, Chulmin Kim
Journal of Korean Medical Science.2023;[Epub] CrossRef
- Bilateral axillo-breast approach robotic total thyroidectomy without isthmectomy: a case report

Original Articles
- Thyroid
- Diagnostic Performance of Thyroid Core Needle Biopsy Using the Revised Reporting System: Comparison with Fine Needle Aspiration Cytology
- Kwangsoon Kim, Ja Seong Bae, Jeong Soo Kim, So Lyung Jung, Chan Kwon Jung
- Endocrinol Metab. 2022;37(1):159-169. Published online February 28, 2022
- DOI: https://doi.org/10.3803/EnM.2021.1299

- 3,882 View
- 164 Download
- 7 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
We aim to validate the diagnostic performance of thyroid core needle biopsy (CNB) for diagnosing malignancy in clinical settings to align with the changes made in recently updated thyroid CNB guidelines.
Methods
We retrospectively analyzed 1,381 thyroid CNB and 2,223 fine needle aspiration (FNA) samples. The FNA and CNB slides were interpreted according to the Bethesda System for Reporting Thyroid Cytopathology and updated practice guidelines for thyroid CNB, respectively.
Results
Compared to FNA, CNB showed lower rates of inconclusive results: categories I (2.8% vs. 11.2%) and III (1.2% vs. 6.2%), and higher rates of categories II (60.9% vs. 50.4%) and IV (17.5% vs. 2.0%). The upper and lower bounds of the risk of malignancy (ROM) for category IV of CNB were 43.2% and 26.6%, respectively. The CNB subcategory IVb with nuclear atypia had a higher ROM than the subcategory without nuclear atypia (40%–62% vs. 23%–36%). In histologically confirmed cases, there was no significant difference in the diagnostic performance between CNB and FNA for malignancy. However, neoplastic diseases were more frequently detected by CNB than by FNA (88.8% vs. 77.6%, P=0.046). In category IV, there was no difference in unnecessary surgery rate between CNB and FNA (4.7% vs. 6.9%, P=0.6361).
Conclusion
Thyroid CNB decreased the rate of inconclusive results and showed a higher category IV diagnostic rate than FNA. The revised guidelines for thyroid CNB proved to be an excellent reporting system for assessing thyroid nodules. -
Citations
Citations to this article as recorded by- Examining the impact of several factors including COVID‐19 on thyroid fine‐needle aspiration biopsy
Muzaffer Serdar Deniz, Merve Dindar
Diagnostic Cytopathology.2024; 52(1): 42. CrossRef - Consensus SFE-AFCE-SFMN 2022 sur la prise en charge des nodules thyroïdiens : intérêt et place de la cytologie thyroïdienne
Myriam Decaussin-Petrucci, Beatrix Cochand Priollet, Emannuelle Leteurtre, Frédérique Albarel, Françoise Borson-Chazot
Annales de Pathologie.2024; 44(1): 20. CrossRef - A comparative analysis of core needle biopsy and repeat fine needle aspiration in patients with inconclusive initial cytology of thyroid nodules
Xuejiao Su, Can Yue, Wanting Yang, Buyun Ma
Frontiers in Endocrinology.2024;[Epub] CrossRef - Preoperative Risk Stratification of Follicular-patterned Thyroid Lesions on Core Needle Biopsy by Histologic Subtyping and RAS Variant-specific Immunohistochemistry
Meejeong Kim, Sora Jeon, Chan Kwon Jung
Endocrine Pathology.2023; 34(2): 247. CrossRef - 2023 Korean Thyroid Association Management Guidelines for Patients with Thyroid Nodules
Young Joo Park, Eun Kyung Lee, Young Shin Song, Soo Hwan Kang, Bon Seok Koo, Sun Wook Kim, Dong Gyu Na, Seung-Kuk Baek, So Won Oh, Min Kyoung Lee, Sang-Woo Lee, Young Ah Lee, Yong Sang Lee, Ji Ye Lee, Dong-Jun Lim, Leehi Joo, Yuh-Seog Jung, Chan Kwon Jung
International Journal of Thyroidology.2023; 16(1): 1. CrossRef - Reevaluating diagnostic categories and associated malignancy risks in thyroid core needle biopsy
Chan Kwon Jung
Journal of Pathology and Translational Medicine.2023; 57(4): 208. CrossRef - A Matched-Pair Analysis of Nuclear Morphologic Features Between Core Needle Biopsy and Surgical Specimen in Thyroid Tumors Using a Deep Learning Model
Faridul Haq, Andrey Bychkov, Chan Kwon Jung
Endocrine Pathology.2022; 33(4): 472. CrossRef
- Examining the impact of several factors including COVID‐19 on thyroid fine‐needle aspiration biopsy

- Thyroid
- A Multicenter, Randomized, Controlled Trial for Assessing the Usefulness of Suppressing Thyroid Stimulating Hormone Target Levels after Thyroid Lobectomy in Low to Intermediate Risk Thyroid Cancer Patients (MASTER): A Study Protocol
- Eun Kyung Lee, Yea Eun Kang, Young Joo Park, Bon Seok Koo, Ki-Wook Chung, Eu Jeong Ku, Ho-Ryun Won, Won Sang Yoo, Eonju Jeon, Se Hyun Paek, Yong Sang Lee, Dong Mee Lim, Yong Joon Suh, Ha Kyoung Park, Hyo-Jeong Kim, Bo Hyun Kim, Mijin Kim, Sun Wook Kim, Ka Hee Yi, Sue K. Park, Eun-Jae Jung, June Young Choi, Ja Seong Bae, Joon Hwa Hong, Kee-Hyun Nam, Young Ki Lee, Hyeong Won Yu, Sujeong Go, Young Mi Kang, MASTER study group
- Endocrinol Metab. 2021;36(3):574-581. Published online May 26, 2021
- DOI: https://doi.org/10.3803/EnM.2020.943
- 6,303 View
- 268 Download
- 8 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
Postoperative thyroid stimulating hormone (TSH) suppression therapy is recommended for patients with intermediate- and high-risk differentiated thyroid cancer to prevent the recurrence of thyroid cancer. With the recent increase in small thyroid cancer cases, the extent of resection during surgery has generally decreased. Therefore, questions have been raised about the efficacy and long-term side effects of TSH suppression therapy in patients who have undergone a lobectomy.
Methods
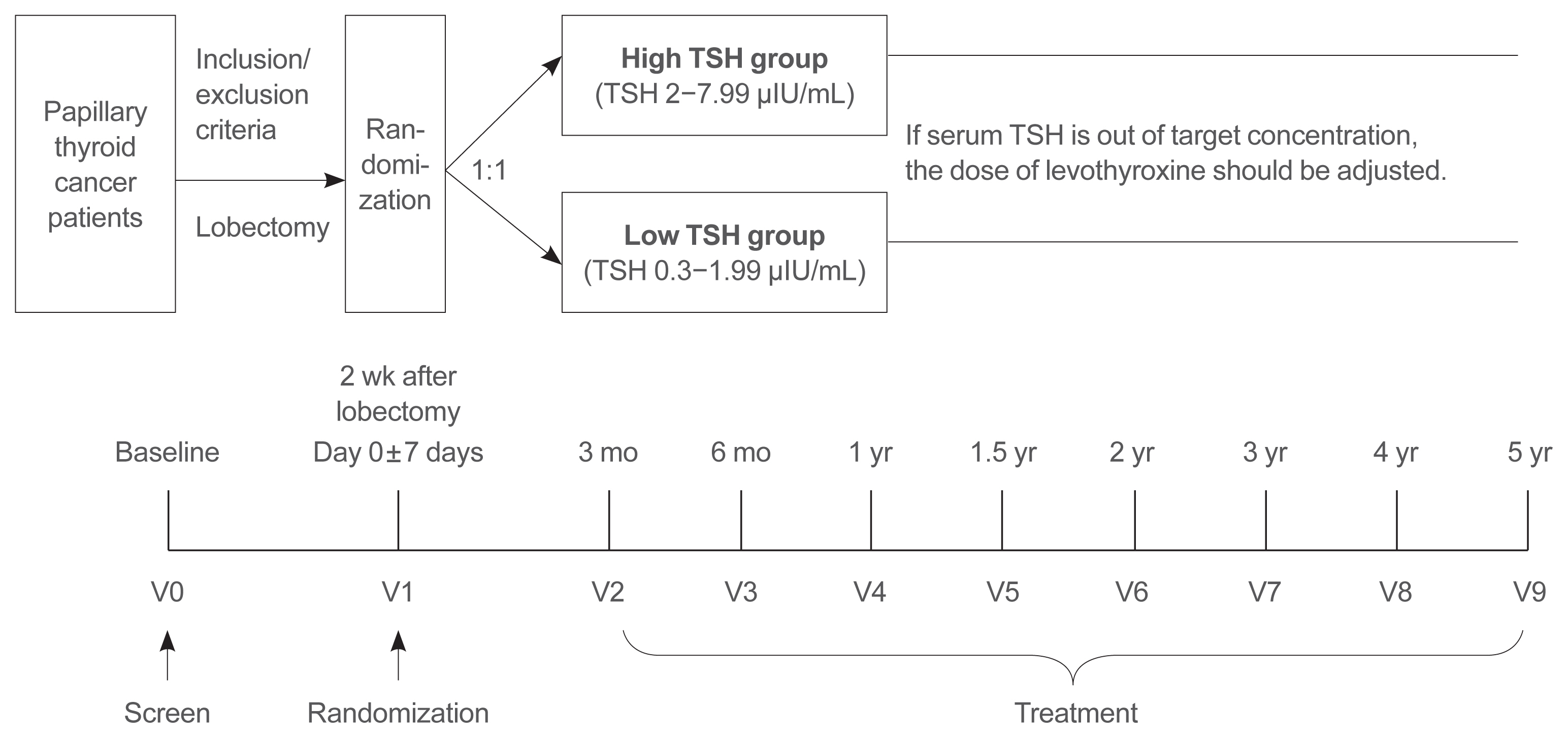
This is a multicenter, prospective, randomized, controlled clinical trial in which 2,986 patients with papillary thyroid cancer are randomized into a high-TSH group (intervention) and a low-TSH group (control) after having undergone a lobectomy. The principle of treatment includes a TSH-lowering regimen aimed at TSH levels between 0.3 and 1.99 μIU/mL in the low-TSH group. The high-TSH group targets TSH levels between 2.0 and 7.99 μIU/mL. The dose of levothyroxine will be adjusted at each visit to maintain the target TSH level. The primary outcome is recurrence-free survival, as assessed by neck ultrasound every 6 to 12 months. Secondary endpoints include disease-free survival, overall survival, success rate in reaching the TSH target range, the proportion of patients with major cardiovascular diseases or bone metabolic disease, the quality of life, and medical costs. The follow-up period is 5 years.
Conclusion
The results of this trial will contribute to establishing the optimal indication for TSH suppression therapy in low-risk papillary thyroid cancer patients by evaluating the benefit and harm of lowering TSH levels in terms of recurrence, metabolic complications, costs, and quality of life. -
Citations
Citations to this article as recorded by- Effect of thyroid-stimulating hormone suppression on quality of life in thyroid lobectomy patients: interim analysis of a multicenter, randomized controlled trial in low- to intermediate-risk thyroid cancer patients (MASTER study)
Ja Kyung Lee, Eu Jeong Ku, Su-jin Kim, Woochul Kim, Jae Won Cho, Kyong Yeun Jung, Hyeong Won Yu, Yea Eun Kang, Mijin Kim, Hee Kyung Kim, Junsun Ryu, June Young Choi
Annals of Surgical Treatment and Research.2024; 106(1): 19. CrossRef - Clinical impact of coexistent chronic lymphocytic thyroiditis on central lymph node metastasis in low- to intermediate-risk papillary thyroid carcinoma: The MASTER study
Da Beom Heo, Ho-Ryun Won, Kyung Tae, Yea Eun Kang, Eonju Jeon, Yong Bae Ji, Jae Won Chang, June Young Choi, Hyeong Won Yu, Eu Jeong Ku, Eun Kyung Lee, Mijin Kim, Jun-Ho Choe, Bon Seok Koo
Surgery.2024; 175(4): 1049. CrossRef - Dynamic Changes in Treatment Response af-ter 131I in Differentiated Thyroid Cancer and Their Relationship with Recurrence Risk Stratification and TNM Staging
璐 狄
Advances in Clinical Medicine.2024; 14(03): 1083. CrossRef - ASO Author Reflections: Active Surveillance may be Possible in Patients with T1b Papillary Thyroid Carcinoma Over 55 Years of Age Without High-Risk Features on Preoperative Examinations
Ho-Ryun Won, Eonju Jeon, Da Beom Heo, Jae Won Chang, Minho Shong, Je Ryong Kim, Hyemi Ko, Yea Eun Kang, Hyon-Seung Yi, Ju Hee Lee, Kyong Hye Joung, Ji Min Kim, Younju Lee, Sung-Woo Kim, Young Ju Jeong, Yong Bae Ji, Kyung Tae, Bon Seok Koo
Annals of Surgical Oncology.2023; 30(4): 2254. CrossRef - Outcomes and Trends of Treatments in High‐Risk Differentiated Thyroid Cancer
Arash Abiri, Khodayar Goshtasbi, Sina J. Torabi, Edward C. Kuan, William B. Armstrong, Tjoson Tjoa, Yarah M. Haidar
Otolaryngology–Head and Neck Surgery.2023; 168(4): 745. CrossRef - Current Controversies in Low-Risk Differentiated Thyroid Cancer: Reducing Overtreatment in an Era of Overdiagnosis
Timothy M Ullmann, Maria Papaleontiou, Julie Ann Sosa
The Journal of Clinical Endocrinology & Metabolism.2023; 108(2): 271. CrossRef - Age-Dependent Clinicopathological Characteristics of Patients with T1b Papillary Thyroid Carcinoma: Implications for the Possibility of Active Surveillance
Ho-Ryun Won, Eonju Jeon, Da Beom Heo, Jae Won Chang, Minho Shong, Je Ryong Kim, Hyemi Ko, Yea Eun Kang, Hyon-Seung Yi, Ju Hee Lee, Kyong Hye Joung, Ji Min Kim, Younju Lee, Sung-Woo Kim, Young Ju Jeong, Yong Bae Ji, Kyung Tae, Bon Seok Koo
Annals of Surgical Oncology.2023; 30(4): 2246. CrossRef - Potential impact of obesity on the aggressiveness of low- to intermediate-risk papillary thyroid carcinoma: results from a MASTER cohort study
Mijin Kim, Yae Eun Kang, Young Joo Park, Bon Seok Koo, Eu Jeong Ku, June Young Choi, Eun Kyung Lee, Bo Hyun Kim
Endocrine.2023; 82(1): 134. CrossRef - Differentiated thyroid cancer: a focus on post-operative thyroid hormone replacement and thyrotropin suppression therapy
Benjamin J. Gigliotti, Sina Jasim
Endocrine.2023; 83(2): 251. CrossRef - Thyroid stimulating hormone suppression and recurrence after thyroid lobectomy for papillary thyroid carcinoma
Mi Rye Bae, Sung Hoon Nam, Jong-Lyel Roh, Seung-Ho Choi, Soon Yuhl Nam, Sang Yoon Kim
Endocrine.2022; 75(2): 487. CrossRef - The Concept of Economic Evaluation and Its Application in Thyroid Cancer Research
Kyungsik Kim, Mijin Kim, Woojin Lim, Bo Hyun Kim, Sue K. Park
Endocrinology and Metabolism.2021; 36(4): 725. CrossRef
- Effect of thyroid-stimulating hormone suppression on quality of life in thyroid lobectomy patients: interim analysis of a multicenter, randomized controlled trial in low- to intermediate-risk thyroid cancer patients (MASTER study)

Case Report
- Pregnancy-induced Osteoporosis Combined with Multiple Compression Fractures: A Case Report.
- Ji Eun Lee, Jin Sun Jang, Sun Hee Ko, Min Hee Kim, Dong Jun Lim, Moo Il Kang, Bong Yun Cha, Sook Hee Hong, Ja seong Bae, Kyeoung Sik Ryu
- Endocrinol Metab. 2011;26(2):150-154. Published online June 1, 2011
- DOI: https://doi.org/10.3803/EnM.2011.26.2.150
- 2,079 View
- 28 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Pregnancy associated osteoporosis (PAO) is a rare condition. It may affect women during pregnancy or after the delivery and it can induce severe back pain. Physicians can find multiple compression fractures on the plain images of these patients. However, little is known about PAO, including the prevalence, the cause, the risk factors and the prognosis. Herein we report on a case of PAO in a 38-year-old female who suffered from severe back pain induced by multiple vertebral compression fractures. After excluding the possibility of unknown malignancy, the patient underwent vertebroplasty to improve the clinical symptom. The bone biopsy results confirmed multiple benign acute compression fractures. The patient was treated with oral bisphosphonate, calcium and vitamin D. She showed clinical improvement without developing any additional vertebral fracture. When young women during pregnancy or just after the delivery complain of persistent back pain, PAO should be considered in the differential diagnosis, and early recognition and treatment are needed for PAO.
-
Citations
Citations to this article as recorded by- Effect of teriparatide on pregnancy and lactation-associated osteoporosis with multiple vertebral fractures
Eun Yeong Choe, Je Eun Song, Kyeong Hye Park, Hannah Seok, Eun Jig Lee, Sung-Kil Lim, Yumie Rhee
Journal of Bone and Mineral Metabolism.2012; 30(5): 596. CrossRef
- Effect of teriparatide on pregnancy and lactation-associated osteoporosis with multiple vertebral fractures


 KES
KES

 First
First Prev
Prev



